
- FR
- EN

In 2017 I wrote an article on how the use of modulators could potentially lead to a shift in how we approach Cystic Fibrosis (CF) from an underwriting perspective. At the time modulators had been around for approximately 5 years and were offering promising outcomes for the select CF sufferers who were fortunate enough to be eligible for the drugs. I wrote about the future of CF being bright and how the insurance industry may need to refine its underwriting approach to the condition, which, was falling into the ‘uninsurable’ category for the most part.
So, have things moved on from 2017? In short, yes! Just this year, the National Institute for Health and Care Excellence (NICE) issued a final guidance securing permanent access to the modulators after lengthy discussions and negotiations between NHS, Vertex and NICE. Equally in 2023, the European Commission granted approval for the expansion of Kaftrio for treatment in Ireland. Modulators in particular Kaftrio, (Trikafta) are now available to those aged two and above in both the UK and Ireland. This article will provide some detail as to how the modulators are having a significant improvement on quality of life and life expectancy. I will also provide an insight into my family’s personal journey with CF and the impact the modulators have had upon my 13-year-old daughter who was diagnosed with Cystic Fibrosis at four weeks old.
To fully appreciate the impact of these new therapies, one must understand the complexities of Cystic Fibrosis, so let us have a recap on what CF is.
CF is a genetic disease that primarily affects the lungs and digestive system although it is associated with other co-morbidities. It is caused by the genetic mutation of the CFTR (Cystic Fibrosis transmembrane conductance regulator), a gene that provides instructions for making a protein that functions as a channel across the membrane of cells that produce mucus, sweat, saliva, tears, and digestive enzymes. In CF there is absent or deficient CFTR production. As a result, the movement of salt and water in and out of cells is not regulated and results in the production of thick sticky mucus. This thick sticky mucus builds up in many of the body’s organs, especially the lungs and the pancreas which causes chronic lung infection, deterioration of lung function and gastrointestinal issues. Pancreatic insufficiency is the most common gastrointestinal complication of CF affecting approximately 85% of CF sufferers. This means that the exocrine pancreas no longer functions sufficiently to digest food and requires pancreatic enzyme replacements for digestion and survival into childhood and adulthood. CF is a life-limiting condition for which there is no cure.
It follows an autosomal recessive pattern requiring both parents to carry the faulty gene. A person must inherit two copies of a defective CF gene, one from each parent to be born with the condition. The gene responsible for CF was first found in 1989 and since then more than 2000 mutations have been identified, however, only approximately 50 mutations are the most common.
Whilst I have described what CF is in literal medical terms, from a personal perspective CF has been a complex condition which has many facets and manifests itself in a host of symptoms. With each pulmonary exacerbation, the lungs are damaged to some extent eventually leading to bronchiectasis and declining FEV1 over time. Not only are there ongoing challenges of maintaining healthy lungs and dealing with gastrointestinal issues such as intestinal blockages and gastroesophageal reflux disease (GERD), but there is also a risk of developing CF diabetes by adolescence. Other complications can include liver disease, nasal and sinus disease and osteopenia owing to lack of absorption of fat-soluble vitamins due to pancreatic insufficiency. Fortunately, the modulators are so impactful that they are, in some cases, reversing pancreatic insufficiency and CF diabetes (reversal of pancreatic insufficiency is seen mainly in very young patients starting the modulators early in life).
I also previously wrote about the challenges in combating pulmonary exacerbations with oral and IV antibiotics (hospital admissions) steroids, anti-fungal treatments to name a few, most of which continues for weeks, possibly months at a time and resulting in horrible side effects.
In addition, physiotherapy or airways clearance is also key in the management of CF required twice daily at minimum. Furthermore, maintaining a healthy BMI is crucial for fighting infections and is also linked to healthier lung status. Pre modulators, this was not always easily achievable in those with CF, and it was a challenge to keep BMI in a healthy range.
The landscape of CF treatment dramatically shifted with the introduction of CFTR modulators; a class of drug designed to correct the malfunctioning CFTR protein at the cellular level. These groundbreaking therapies target the underlying genetic mutation, and the focus is no longer on treating downstream effects of the condition i.e. its symptoms and complications. Essentially the modulators improve the production and processing of CFTR proteins. When the CFTR proteins are more effective the chloride flow between cells is restored or improved such that it can relieve symptoms of CF.
Modulators were first introduced in 2012 to treat those with G551D mutation and over the last 12 years we have seen the introduction of other modulators that treat those with at least one copy of the Delta 508 mutation. This mutation is the most common genotype in the UK and Ireland, with almost 90% of CF sufferers carrying at least one copy of the mutation. As mentioned already, we have seen accessibility to Kaftrio, the newest drug available and perhaps arguably the most effective yet, being granted to those aged 2 and above.
Modulators are reshaping the lives of those living with CF by providing significant improvements in pulmonary and extrapulmonary outcomes and modifying the course of the disease by slowing progression and improving survival. Clinicians are seeing patients with a reduction in pulmonary exacerbations, improved lung health, improved nutritional status with increasing BMIs, increased energy and activity having a positive effect on general wellbeing. Equally the time spent in hospital for those with CF is also reducing.
This is borne out in the data from the most recent UK CF registry annual data report (2023). Firstly, there are more people now living with CF; the report states 11,319 registered people compared to 10,810 in 2015. At that time there were 59.9% aged 16 years and over (adult patients) compared to 68% in 2023 showing that the adult population is growing due to low mortality in children and increasing longevity in adults.
Looking at FEV1s from the 2023 annual report, there is a significant improvement in recorded readings:
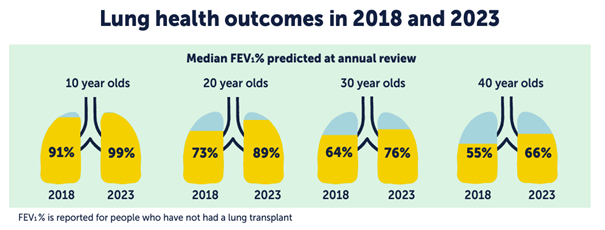
From experience, any upward shift in FEV1 is a very welcome outcome for the CF sufferer and the family but to claw back 12 or 16% in FEV1 levels (as seen in 20- & 30-year-olds) would have been a miracle some years ago. FEV1 is the main marker for benchmarking continuing lung health. These are phenomenal outcomes! If we then review IV treatments, we can also see a very positive outcome in 2023 with admissions halved since 2018.
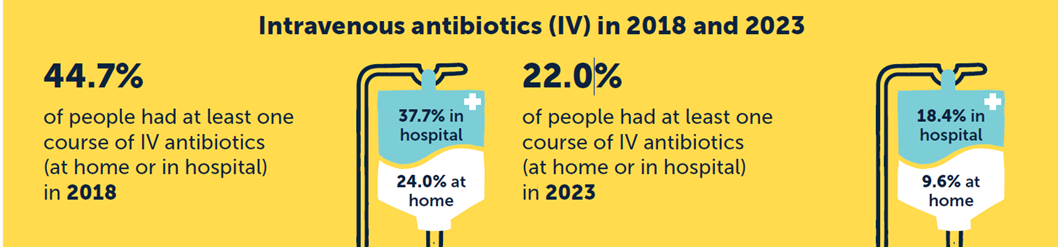
IV treatments are generally a minimum of 2 weeks, with intense doses of IV antibiotics administered several times a day accompanied by intense physiotherapy daily. They can have a psychological and physical impact on those with CF. As one can imagine any reduction in the need for IV treatment is hugely positive.
Effects of the modulators on those commencing the drugs at much younger ages are starting to play out in clinical settings with some children not requiring the need for pancreatic enzyme replacement drugs due to pancreatic insufficiency being reversed. From personal experience, this alone is a game changer and eliminates the need for children to take up to 20/30 tablets a day. Pancreatic enzyme replacement drugs are given with every meal or snack to ensure digestion of food which is essential for healthy BMIs.
In addition, modulators are reversing symptoms of CF diabetes in those either on the cusp of diagnosis or early diagnosis i.e. those in adolescence. The number of 10 to 15 years old with CF diabetes dropped from 10.4% in 2018 to 8.1% in 2023. This is yet another positive aspect of how the modulators are having a significant impact on the treatment of CF.
At the time of publishing my first article, the median predicted survival for CF sufferers was approximately age 47. Median predicted survival as indicated in the 2023 UK CF registry annual report stands at age 64, a dramatic upward shift. The result of a simulation model published in the Journal of Cystic Fibrosis in July 2023 showed the median projected survival for patients with CF homozygous for F508del- CFTR (the most common form of CFTR mutation among patients with CF) treated with Kaftrio was 71.6 years. The most recent modulator Kaftrio, which by all accounts has shown the most promising outcome, is relatively new having only been available in recent years so there is hope that new generations of CF sufferers will potentially have near normal life expectancy.
Whilst having been diagnosed at four weeks old, she did not require IV treatment until she was two years old and following that there were several infections (pulmonary exacerbations) each year with some requiring inpatient treatment. By the time she was about six, she developed ABPA (Allergic Bronchopulmonary Aspergillosis), a fungal infection which required three months steroids along with anti-fungal meds at a time. For her, it recurred time and time again. Periods of perhaps a few months of her being well would be blighted by another pulmonary exacerbation, whether it be a bacterial chest infection or ABPA. The treatment regime when she was well was intense and could take several hours a day – this involved nebulised antibiotics, nebulised mucolytics, airways clearance, bronchodilators, laxatives daily for tummy issues and Creon. When she was unwell, treatments increased with addition of new antibiotics, steroids etc for protracted periods and possible inpatient treatment. CF can be all consuming at times; there is never a day off from CF. In everything we did, CF was forefront in our minds. The smallest of things, like school meals had to be carefully planned to ensure she had the correct dosage of her Creon.
By 2021 her journey changed direction and not for the good; she was diagnosed with NTM abscessus (Non-tuberculosis Mycobacterium) which is an incredibly difficult bacteria to eradicate. Treatment plans last up to two years and clinical outcome can be poor if the bacteria are not eradicated. This was also complicated by a yet another exacerbation of ABPA and a resurgence of Pseudomonas aeruginosa for which she has been on lifelong nebulised antibiotic, Colomycin. Much of 2021, she spent having IV of some form, antibiotics, steroids. Hospital stays, appointments, and tests were a constant. Her lung function showed some improvement but not what we or her team had hoped for. Towards the end of 2021 her appetite was diminished, and her weight had plummeted such that we were discussing insertion of a feeding tube in January 2022. She was losing her hair from the combination of treatments, and she had presented with haematuria and glycosuria. These were just a few of the side effects from the treatments. It was a constant battle of treating the infections, trying to improve her lung function whilst combating the side effects which were hindering her wellbeing and causing added problems. It was by far the most challenging year for her and us as a family with her CF journey. She was already taking the modulator Symkevi, which was not showing much in the way of improvement for her. We were exhausted, emotionally drained and hope was really faltering! Her team were phenomenal, but we all knew that she would benefit greatly from the new modulator Kaftrio which was not available to under 12s at the time (she was 10). By this point, she had become a high focus case for her CF Team.
By January 2022, the news broke that Kaftrio was to be licenced to age 6- to 12-year-olds and it was a matter of weeks before her life and our family life would alter so spectacularly. It is beyond words what the modulators have done for us. Within four weeks of starting the drug Kaftrio, she was a different child, full of energy, enjoying her food with finally having a healthy FEV1. And she has remained very well since, having not required any IV treatments since December 2021. In fact, she eradicated NTM and has not grown Aspergillus or any significant bacteria since 2021. The burden of treatments has reduced considerably, and we are now considering the cessation of some other treatments. Kaftrio has been truly transformative for my daughter and our family, and our story is testament to the incredible benefits of using modulators.
The advent of modulators is changing the natural history of this disease and the younger generations with CF who will enter the insured population in the coming years will have significantly improved life expectancy. I believe we need to examine our current guidance on CF to ensure that we are committed to our societal responsibility as insurers by insuring as many lives as possible on equitable terms. Even those who have lived with CF for many years without modulators are having such positive responses to the drug, that underwriting terms may be possible with some restrictions.
Research remains key to the advancement of medical therapies and establishing new treatment options for treating those not eligible for modulators which is approximately 10% of CF sufferers. There is much research under way in areas such as gene therapies, phage treatments and antimicrobial resistance and studies looking at the longer-term effects of the CF modulators as well as how to manage an ageing CF population. Early phase genetic therapy clinical trials are now recruiting a few people with CF in the UK which is incredibly important and holds much promise for the future.
Clinical trials of next generation CF modulator Vanza, a new triple combination modulator has shown to have added benefits when compared to Kaftrio. The company responsible for developing all CF modulators are currently submitting a licence application for this therapy to be used in people with CF aged six and over.
With such advancements and breakthroughs and a continued improvement in survival, the future for people with CF is promising.
